Vein Transpositions
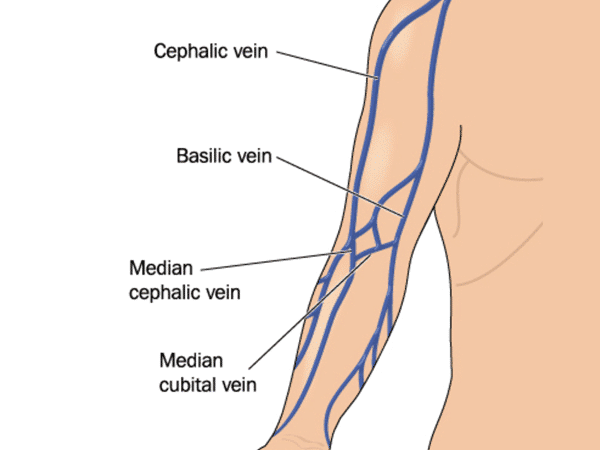
For patients who require Hemodialysis, a properly functioning vascular access is crucial for achieving optimal quality of life. If a suitable cephalic vein at the forearm and upper arm cannot be found, an arteriovenous fistula (AVF) is made using a prosthetic graft or a transposed basilic vein. The latter is completely protected from venipuncture owing to its deep position in the subfascial plane.
Basilic vein transposition (BVT) was first performed in 1976 and is considered a viable option for secondary or tertiary vascular access. Fistulas made with a transposed basilic vein have been found to be the most reliable secondary vascular access procedures for chronic Hemodialysis.
Conventional BVT
In Conventional Basilic vein transposition (BVT), a long incision is made over the medial aspect of the arm. The basilic vein is dissected up to the axillary vein and transposed into the subcutaneous tissue using multiple small incisions, followed by End to side basilic vein brachial artery anastmosis.
Transposition of Basilica Vein with Minimal Incision
In this process, performed under local or regional anaesthesia, a transverse skin incision is made on the antecubital area to identify a basilic vein and brachial artery. Following this, three or four longitudinal skin incisions are made along the basilic vein, which is is then pulled out toward the axillary region. With the help of a tunneler, tunneling is performed under the skin and the full length of the basilic vein is transpositioned towards the lateral side of the upper arm. End to side basilic vein brachial artery anastmosis then conducted, with a small or minimal incision applied to basilic vein transposition to lessen the pain and make patients more comfortable.

